Hip Replacement
Hip replacement surgery is very common. According to the 17th Annual Report of the National Joint Registry published in 2020, over the three years from 1st January 2017 to 31st December 2019, 281, 196 primary hip replacements were performed by 2,303 surgeons working in 420 units across England, Wales and Northern Ireland.
Prior to the Covid pandemic we performed approximately 300 hip replacements per year.
Hip replacement surgery involves replacing the arthritic hip joint with an artificial joint. This is also known as a prosthetic joint.
The socket in the pelvis, known as the acetabulum is excised and an artificial hemispherical prosthetic socket commonly known as a cup is then inserted into the pelvis.
The ball part of the joint, the head of the femoral bone, is removed. A prosthetic stem is then inserted into the femur (thigh bone) A new ball is then attached to this stem to create the new ball and socket joint.
The new socket and stem are held in place either by a special material attached to the surface of the prosthesis which allows your own bone to grow onto this surface and fix it in place, or else a surgical cement is used to glue them in position. This is very similar to that used in dental surgery to fix metal fillings in place.
The ball, stem and socket can be made from a variety of materials such as metal, plastic and ceramic.
There are numerous hip replacements produced by a variety of manufacturers. In 2011, 142 brands of femoral stem and 119 brands of acetabular cups were available.
We only use prosthetic components with a proven track record. The hip prostheses we use in over 99% of cases are either the Exeter – a stem requiring cement, or the uncemented Accolade II and Corail stems. We have both visited the design centres for these prostheses and learnt the specific surgical techniques for their insertion.
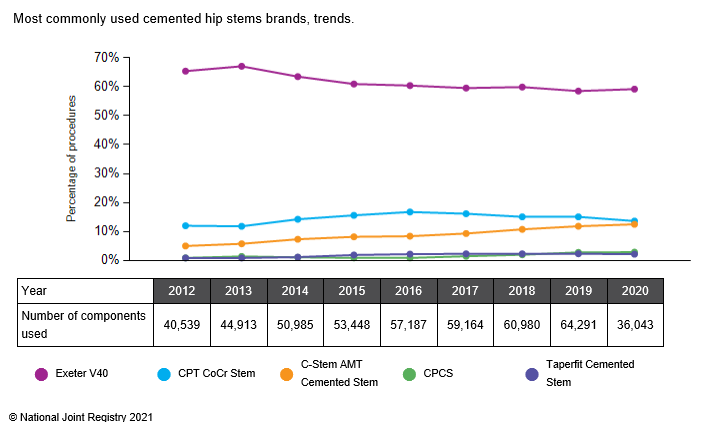
The Exeter stem, designed in Exeter England and currently manufactured by Stryker, is a stem that requires insertion of a grout/cement. It is the most commonly used cemented stem, accounting for 60% of all those used as shown in the graph below.
An example of a cemented right Exeter Hip Replacement is shown next to the R marker on the left side of the X-ray image. The normal left hip is shown in the right side of the picture.

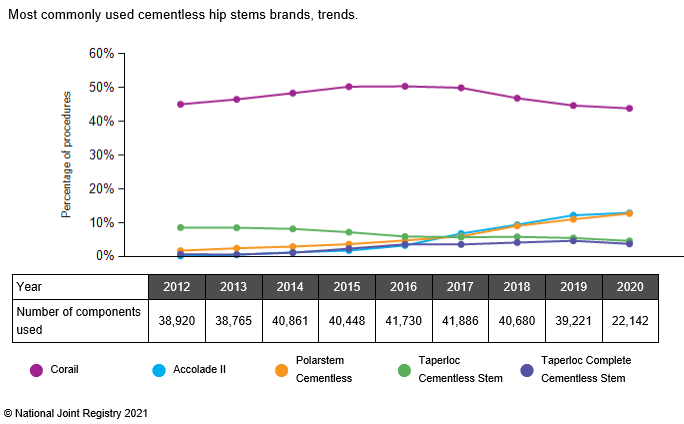
We also use both the Accolade II and the Corail stem which are uncemented stems. The Corail was designed in France and is manufactured by Depuy, whilst the Accolade II is manufactured by Stryker. These are the most commonly used cementless stems used in the UK, as seen in the chart below,
An x-ray of the Corail stem:

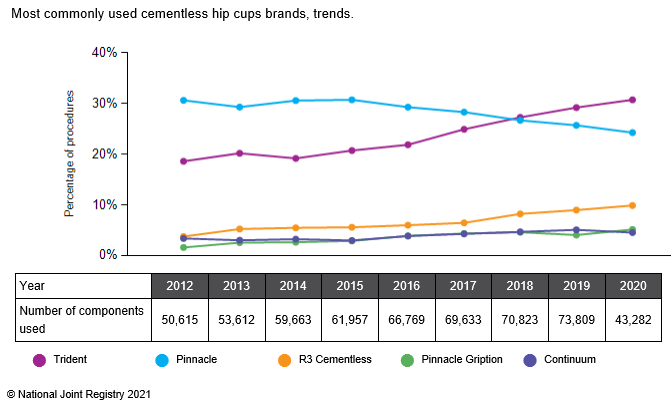
The implants we use for your new acetabulum (known as a cup) are in the majority of cases either the Trident (manufactured by Stryker) or Pinnacle (manufactured by Depuy) which are the most commonly used uncemented cups in use in the UK. In 2018 the Trident became the most commonly used cementless hip cup, accounting for 27% of those used. Having been the market leader for a number of years the Pinnacle became the second most widely used brand in 2018.
The combination of an Exeter stem with a Trident cup have excellent survival rates as shown by the results in the national joint registry (18th report published 2021) which reveal that since 2003 of 110, 306 Exeter trident hips implanted the revision rate at 17 years is 4.06%. This means that seventeen years after the hip has been implanted the chances of you requiring a revision procedure is less than 5%.
For both Accolade II/Trident and Corail/Pinnacle hips the revision rates at 5 years are 1.81% and 2.14% respectively.
A Trident cup. This is inserted into your pelvis. Into this is inserted either a plastic or ceramic liner which articulates with the new ball on the stem, as is shown in the second picture.

The final consideration in your hip replacement will be the articulation between the new ball and socket. The balls can be made from metal or ceramic and the sockets can be made from metal, ceramic or plastic. We do not perform hip replacements using metal on metal bearings.
The choice of bearing surfaces will be discussed at your consultation.
Further Information on the prostheses discussed above which we use for your hip replacement can be found in the links below:
Preparing for Joint Replacement Surgery
If you are considering having joint replacement surgery this is a useful aid to help you understand the risks and benefits of joint replacement surgery.
Further information and patient experiences of using the aid can be found at
https://www.njrcentre.org.uk/njrcentre/Patients/Patient-Decision-Support-Tool
Undertaking exercises prior to your surgery has benefits and can help to make your surgery more successful. A useful video produced by the American Association of Hip and Knee Surgeons can be found here
Preparing for Joint Replacement Surgery: At-Home Exercises
Procedure for Hip Replacement Surgery
Once it is decided you need a hip replacement, prior to the actual surgery there are a number of things that take place to ensure that the operation proceeds as smoothly as possible and that you are well prepared following discharge from hospital back home with your new hip replacement.
Pre-operative assessment
Prior to the surgery you will attend a preoperative assessment clinic. This is to ensure you are fit enough to undergo the surgery. You will be asked questions regarding your general health and current medications that you take by a specialist nurse and/or anaesthetist. Following this your blood pressure will be checked and your heart and chest will be examined.
A blood sample will be taken as well as a urine specimen. A special examination of the heart known as an ECG will also be performed. Additionally a chest X-ray may be performed.
You will also be seen by a physiotherapist and occupational therapist. This is an ideal opportunity to ask questions about any concerns that you may have about getting around at home following your discharge home. Such concerns commonly include asking about rearranging your furniture to enable you to get about your house more easily after the surgery, removing any rugs/mats which could pose a risk to you slipping/falling, moving items so that they are within easy reach and avoiding you having to bend down/reach up.
The occupational therapist may arrange for specialist equipment to be available to help you at home following discharge. This may include installation of such items as:
Stair rails, raised toilet seats, shower chair and the provision of assistant devices such as a long handled shoe horn, or long handled grabbing tool to avoid bending over.
You will also be assessed for your consent to allow your personal details to be held by the National Joint Registry. This is voluntary but extremely useful. The details of all prosthetic hip, knee, shoulder, elbow, and ankle implants which are implanted are submitted to the NJR and submitting your details allows us to track and monitor the outcomes of these. More information can be found here: https://www.njrcentre.org.uk/njrcentre/Patients
Day of surgery
You will be provided with a carbohydrate drink to take the evening before and six hours before your planned surgery.
You are usually admitted on the day of your operation. Your surgeon and anaesthetist will see you prior to your operation and answer any last minute questions/concerns you may have. Prior to going to the operating theatre you will receive Gabapentin and Oxycontin (pain relieving medication).
The anaesthetic we prefer to use for your surgery is that of spinal regional anaesthesia. This has been shown to reduce the amount of blood loss during surgery and possibly reduce the complications from blood clots following your surgery. It also avoids the insertion of a tube into your throat which is required with a general anaesthetic. This can give you a sore throat for a few days following surgery. Nausea, drowsiness and headaches which are common problems with general anaesthesia are also avoided.
The spinal anaesthesia involves injecting a small amount of anaesthetic into the fluid surrounding the spinal cord in the lower back. This induces a short acting loss of sensation (numbness) in your lower limbs which allows the operation to take place pain free. The feeling returns to your legs after a few hours, after the operation has been completed.
This process is undertaken in the anaesthetic room and then you are then moved to the operating room next door. Sedative medication is also administered at this time if needed.
The anaesthetic will be discussed preoperatively with your anaesthetist. If there are any contraindications to undergoing a spinal anaesthetic then you will be offered a general anaesthetic.
Antibiotics to reduce the risk of infection and a drug to reduce post operative bleeding (Tranexamic acid) are given prior to surgery starting.
The surgery itself is undertaken in a specially designed operating theatre to reduce the risk of infection. This is known as a laminar air flow theatre.
You will be placed on your side on the operating table and held there with specially designed supports placed on your back and front of your pelvis. Your skin is then shaved if necessary and disinfected prior to surgery, again to reduce the risk of infection.
At the end of the operation local anaesthetic is injected into the tissues around the hip joint, to reduce post operative pain.
A routine hip replacement is usually performed in 1-1 ½ hours. You will spend some time in the theatre recovery room prior to being transferred back to the ward. The whole process of leaving and returning to your ward usually is about three hours.
Post operative care
Usually the day after your operation, sometimes the same day, you will start your rehabilitation by getting up out of bed and walking with the help of the physiotherapist. Following the hip replacement you are normally able to put all of your weight through your new hip. If there is any reason why you can’t, your surgeon will indicate this and explain why.
Initially you may need the use of a special walking frame (a zimmer frame) but should quickly progress to using walking sticks.
Blood tests will be taken following your surgery and you will have an X-ray taken of your new hip replacement.
Blood thinning injections will be given into your stomach whilst you are in hospital to reduce the risk of you developing a blood clot in your veins. When you are discharged you will be given some tablets called Rivaroxaban which you will need to take daily up to five weeks following your surgery to continue to reduce your risk of developing a blood clot. You will also be provided with some special stockings to wear which are also designed to reduce this risk.
Analgesic medication is provided to reduce the postoperative discomfort and ensure you are able to undertake the required physical therapy to ensure a rapid return to normal mobility.
The majority of our patients are discharged within four days of their surgery. It is usual to be discharged when you can walk safely with two walking sticks including going up and down a flight of stairs.
What can I expect after my Hip Replacement?
Once at home following discharge from hospital you should keep your wound dry until your stitches/skin clips have been removed. These will usually be removed about ten days following your surgery.
If any redness develops around your scar, or it continues to leak fluid, you should either consult your GP or your surgeon for advice.
Following your hip replacement, you should expect a reasonably quick return to your lifestyle and activities without the pain and aching that you experienced prior to the hip replacement. Specific concerns commonly include the following
When can I sleep on my side/stomach?
We usually advise you to sleep on your back for the first four weeks following your surgery. Following this period sleeping positions are unrestricted.
When can I get in a car and when can I drive?
Following your hip replacement you can sit in a car when you are discharged from hospital. We recommend however that you avoid travelling in cars with low fitting seats for at least four weeks following your surgery.
We advocate avoiding driving until four weeks after your surgery. You need to ensure that you can perform an emergency stop and hold your foot on the brake (and clutch) for at least 10 seconds.
When can I cross my legs or bend down at the waist?
You should avoid crossing your legs or bending down at the waist for the first four weeks following your surgery
When can I have sexual intercourse
Sexual activities can usually be resumed within four weeks after your surgery. Any concerns with this should be discussed with your treating surgeon. More useful information can be found here https://hipknee.aahks.org/a-guide-to-returning-to-sexual-activity-following-total-hip-and-knee-replacement/
When can I resume sporting activities, dancing or gardening?
This depends upon the sporting activity in question. Swimming can be resumed once the wound is healed, as can activities such as walking, golf and dancing.
Gardening activities that avoid bending at the waist can be resumed once the wound has healed. You should avoid bending down as mentioned above for four weeks following your surgery.
Activities that involve impact stresses on the joint such as jumping, jogging and contact sports should be avoided following your hip replacement.
Airport Security
We commonly get asked about whether your new hip implant will set off the detectors at the airport. The American Association of Hip and Knee Surgeons have produced a useful video which can be found here https://www.youtube.com/watch?v=7hagY2S9l3k&feature=emb_logo
Further information can be found in the link below:
What are the risks?
Hip replacement surgery is a major operation. Complications albeit rare can occur. You should be aware of these risks prior to consenting for your operation. The statistics quoted are national figures.
General complications related to surgery
Deep vein thrombosis (about 3%): This is a blood clot in the deep veins of the legs, and/or thighs. Rarely part of this blood clot can dislodge and travel to and become lodged in the lungs causing a pulmonary embolism (less than 1%) This is a serious and potentially fatal condition.
We try and reduce this risk by using special equipment during your operation to regularly and intermittently gently squeeze the calf muscles of your other leg. This is known as a flowtron gaiter. Post operatively you will receive blood thinning medication, and will be given TED stockings to wear.
Urinary problems. Occasionally you will have problems urinating after surgery. This may necessitate insertion of a temporary urinary catheter, which is usually removed when you are up and fully mobile – usually a few days at most.
Nausea, loss of appetite and constipation. These are common after surgery. They usually resolve after two or three days. Stool softeners may be prescribed if you develop constipation.
Cardiorespiratory complications such as a heart attack, stroke or chest infection (less than 1%) Prior to your surgery your fitness to undertake the hip surgery will be assessed to try and reduce this risk.
Complications due to hip surgery
Dislocation (less than 1%): The ball can dislocate from the socket. The highest chance of this happening is in the first six weeks following your operation until all of the tissues around the hip joint have healed. Your physiotherapist will guide you on how to reduce this risk following your operation.
Deep Infection (less than 0.1%) Following your operation occasionally the wound can leak some fluid. This usually settles after a few days. A superficial infection can occur which usually responds to oral antibiotics. Infection however can sometimes occur deep in the hip joint itself around your new hip prosthesis. This may occur at any time after your operation, sometimes many months or years after your operation. If this deep infection does not respond to antibiotics there is a risk that you will need to undergo a further operation to replace this infected hip.
Nerve injury. This is very rare (less than 1 in 1000). It may result in foot weakness (foot drop) necessitating the use of a special splint.
Leg length difference. Sometimes the surgery will result in a slight difference in your leg lengths. This can be disabling and require the use of an insert in your shoe to equal your leg lengths out. We minimise this risk and carefully check your leg lengths intraoperatively.
Fracture of the thigh or pelvis. (less than 1%): This rare complication can ne treated during the operation but may require you to walk using crutches for several weeks after the operation to allow the fracture time to heal.
Ankle swelling. This is very common and usually takes several months to resolve. Squeaking. Audible noises following a hip replacement have a prevalence which ranges from 0.66% to 7.0% in published articles. The audible noise usually develops more than a year after surgery. There are multiple factors associated with this.
Get News & Updates
Stay in the loop with Northampton Orthopaedics with our latest news, events and advice.
What Patients Say

