Knee Treatments
Northampton Orthopaedics deliver a range of Knee Treatments to patients across Northamptonshire and beyond. These include non-surgical treatments, drug treatments and surgical treatments.
Covered on this page:
- Non Surgical Treatment Following Acute Knee Injury
- Exercise and Physical Therapy
- Non Surgical Treatment of Arthritis
- Lifestyle Modification and Exercise
- Braces & External Supports
- Analgesics and Anti-inflammatory Drugs
- Corticosteroids
- Viscosupplementation
- Arthroscopic Knee Surgery
- Meniscal Knee Surgery
- ACL Reconstruction
- Other Ligament Reconstructions
- Cartilage Surgery
- Knee Arthritis Surgery
- Knee Osteotomies
- Partial Knee Replacement
- Total Knee Replacement
Non-Surgical Knee Treatments
Non-Surgical Treatment Following Acute Knee Injury
The majority of knee injuries get better without the need for any surgical intervention. Knee knocks and strains usually require initial treatment with “RICE” – Rest, Icing, Compression and Elevation, followed by a gentle return to activity. Often initial pain and discomfort can be managed with simple pain killers (e.g. Paracetamol) and an anti-inflammatory (e.g. Ibuprofen). It is common for even simple strains and bruises to take several weeks to settle. Inability to bear weight, locking or joint instability are concerning symptoms and further opinion from doctor or sports physiotherapist should be sought.
Occasionally knee braces may be helpful to either hold the knee in a resting position or to help provide stability to the joint as it moves. There are a number of complex (and expensive) braces on the market that can help provide stability following ligament or tendon injuries – these often require expert fitting and advice should be sought prior to their purchase.
Exercise and Physical Therapy
Exercise and physical therapy often helps to rehabilitate the joint and restore power.
Damaged hips and knees often stiffen and weaken as a direct result of under activity. Exercise programmes and physiotherapy can help to restore function through non-surgical means. Personalized exercise and rehabilitation regimes can be developed with the help of sports and physiotherapists.
In addition to physical exercise regimens, some physiotherapists can also provide deep tissue massage, ultrasound therapy, muscle stimulators and other techniques to help speed recovery.
Lifestyle Modification and Exercise
As the symptoms of arthritis become more intrusive it is often necessary to alter activities and lifestyle to help avoid or delay progression of the disease. “Denial” is seldom effective in the longer term!
Weight loss can significantly improve symptoms of pain and instability as the forces (and wear and tear) passing though the joint are dramatically reduced. Unfortunately reduction in weight usually requires eating less (less energy in) as the arthritis symptoms often won’t allow a dramatic increase in exercise.
Higher impact exercises (running, twisting, jumping) should generally be avoided as they tend to precipitate painful episodes. Lower impact exercises (cycling, swimming, cross-trainers etc) help maintain muscle strength, range of movement and cardiovascular fitness without causing as much irritation within the joint.
Braces and External Supports
Many support devices are available to help manage the symptoms of arthritis. The correct use of a walking stick or cane can greatly reduce the force passing through the arthritic joint and improve pain, stability and walking distance.
For certain types of knee arthritis (isolated to one part of the joint) off-loading knee braces can be effective in stabilising the joint and in helping to move force away from the injured area. As with other types of complex knee braces these devices are expensive and require expert fitting to ensure they are positioned correctly.
Drug Treatments
Analgesics and Anti-inflammatory drugs
Simple oral pain killers (analgesics) such as paracetamol and codeine are usually helpful in managing the pain associated with acute knee injury and arthritis. There are vast arrays of analgesics available in different forms, so if one type doesn’t help there are often alternatives available. Stronger analgesics require a prescription – this can be provided following review by a general practitioner or your surgeon.
Non Steroidal Anti-inflammatory Drugs (NSAIDs) e.g. ibuprofen and diclofenac can often be taken with other analgesics to help reduce swelling, inflammation and pain. These medications should be used with caution as they can cause gastrointestinal side effects if taken for a prolonged period. NSAIDS should be avoided in people who suffer from severe asthma or chest problems and in those people with kidney problems – as always, if you are concerned advice should be sought from a medical practitioner.
Corticosteroids
Corticosteroids are powerful anti-inflammatory agents that can be injected into or around joints and muscles.
They can be given to help reduce the pain and swelling produced by inflamed joints and soft tissues. Usually steroid injections are used to treat acute “flare-up” pain associated with mild to moderate arthritis. Steroid injections usually take several days before they begin to improve symptoms and some patients find that the joint may initially become more painful for a short time. The benefit gained from steroid injections varies from patient to patient – typically symptoms are improved for a few months.
There are concerns that prolonged or excessive use of corticosteroids may actually cause harm to the joint and alter the body’s own immune system – their use is usually limited to 2 – 3 injections per year.
Viscosupplementation
Viscosupplementation is an injection treatment to help relieve the pain of knee or hip osteoarthritis. The injection contains HA (Hyaluronic Acid) which is a naturally occurring molecule that helps provide cushioning and lubrication within a normal joint.
The injection is given as an outpatient or day case procedure and usually takes 15 to 20 minutes.
The effects of viscosupplementation tend to be similar to corticosteroid injections – although longer-term benefit has been shown in a number of studies. The treatment is not effective in all cases, and is not helpful in more advanced arthritis.
Surgical Knee Treatments
If conservative or non-surgical management has not improved symptoms then surgical intervention may be beneficial.
Some of the more common types of knee surgery include:The arthroscope is a narrow fibre-optic telescope attached to a camera. Arthroscopy allows the surgeon to directly visualise problems within the joint and often provide treatment using specially designed surgical instruments. Arthroscopic surgery generally allows a faster recovery and produces less post operative pain than more traditional “open” procedures.
Knee arthroscopy is performed for a number of reasons. More common indications include:
- Diagnostic purposes – when previous imaging has not found a cause for a knee problem
- Treatment of damaged meniscal cartilage
- Treatment of damaged articular cartilage
- Removal of loose fragments causing problems in the knee
- Ligament reconstruction procedures
Arthroscopic surgery is usually performed as a day case procedure – meaning the patient enters and leaves the hospital on the same day.
The surgery is carried out in the operating theatre and usually involves a general or regional (epidural or spinal injection) anaesthetic. A tight tourniquet is placed around the thigh prior to the surgery to prevent bleeding during the operation. The majority of operations last less than 45minutes although more complex ligament procedures may take up to 2hours. At the end of the procedure local anaesthetic is put into the wounds to help reduce post operative pain. The wounds are usually closed with paper “Steri-Strips” or stitches.
After the operation and recovery from the anaesthetic, walking can begin – initially with the aid of crutches. A physiotherapist will help and give advice on how to use crutches properly.
Once the patient is comfortable and safely getting about then it is fine to go home, this is normally 2 to 6 hours after the surgery. It is essential that the patient has somebody to drive them home following the operation. Following a general or regional anaesthetic the patient should have somebody stay with them until the next day.
Post operative care
Recovery and rehabilitation advice will vary according to the procedure that has been performed. Details will be provided by the surgeon and physiotherapist following the surgery.
Usually the knee should be rested for the first few days to allow the wounds to settle. It is normal for the knee to swell following arthroscopy and elevation helps to reduce this. Simple pain killers may be needed in the first few days.
The bandage applied after the operation can often be removed and may be replaced with a compression “tubigrip” support bandage – your surgeon will let you know when this should be done. The plasters and strips covering the wound can be removed from 4-7 days. The wounds should be kept clean and dry until they have sealed over. Showering and bathing can begin at this time.
Rehabilitation
In the first few days following arthroscopic knee surgery, simple rehabilitation exercises including straight leg raising, hip, knee and ankle range of movement and thigh muscle strengthening and tightening exercises should be commenced.
Return to activity
Generally, return to activities takes between two and six weeks. Recovery, however, depends on the extent of damage within the knee and the surgical procedures performed.
Approximate recovery times following simple arthroscopic surgery:
Sedentary (office type) work 2-5 days
Physical work 1-3 weeks
Light training 3 weeks
Return to full impact activities 4-6 weeks
Driving 2-4 days once walking comfortably without crutches
What are the risks of arthroscopy?
Knee arthroscopy is commonly performed procedure and is generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
Side-effects
These are the unwanted, but mostly mild and temporary effects of a successful treatment, for example feeling sick as a result of the general anaesthetic.
After a knee arthroscopy you will have small scars on your knee from the cuts. The knee is usually sore for a week or so. The “portal sites” (entry wounds) can often be tender and uncomfortable – especially on kneeling for several months.
Complications
This is when problems occur during or after the operation. Most people aren’t affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, a wound infection, excessive bleeding or developing a blood clot, usually in a vein in the leg (DVT).
Arthroscopy complications can include:
- Infection
- Loss of sensation in the skin over your knee or around the entry wounds
- Bleeding into your joint
- On-going stiffness or pain
- The surgical procedure may not be successful
The exact risks are specific to you and differ for every person.
Meniscal Knee Surgery
Meniscal injuries are one of the more common problems presenting to the knee clinic. If the meniscal damage causes on-going symptoms then surgery may be helpful. The vast majority of meniscal problems are now treated using arthroscopic surgical techniques.
The treatment of a torn meniscus depends upon the location, type and age of the injury.
Menisectomy Procedure
In the majority of cases the torn fragments of loose meniscal cartilage are trimmed or “debrided” away to prevent catching and painful irritation within the knee (menisectomy procedure). This usually allows early return to activities and a relatively short rehabilitation period.
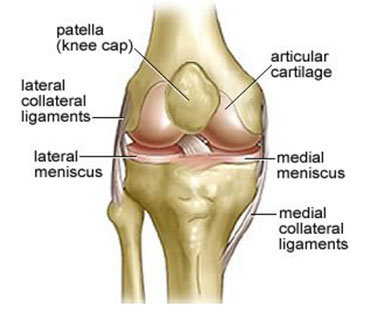
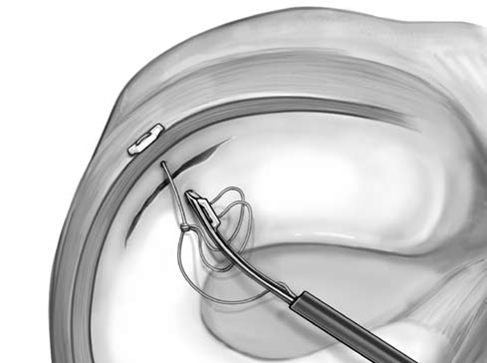
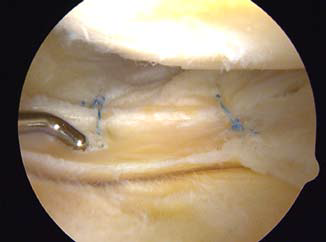
Meniscal Repair Procedure
In some instances the meniscal tear may be amenable to repair. This is more common in acute injures and larger tears in an attempt to preserve the “shock absorbing” functions of the meniscal cartilage.
Meniscal repair is usually performed arthroscopically. Occasionally the procedure may require extra portals or incisions to be made to safely access the injury.
A longer rehabilitation is required following meniscal repair compared with menisectomy. A knee brace is usually worn for six weeks after the surgery – restricting knee flexion to 90 degrees. For three months after repair surgery impact loading activities (running/jumping/twisting) and squatting exercises must be avoided.
The success rate of meniscal repair is in the region of 70%. If the repair fails further surgery may be needed to repeat the repair or remove the loose meniscal cartilage.
Anterior Cruciate Ligament (ACL) Treatment
Anterior Cruciate ligament injury may lead to ongoing instability and giving way symptoms. Surgery is not required for all ACL injuries. Some patients may choose to modify their activities and lifestyle to avoid further knee injury and giving way episodes. Non-operative treatment may help to strengthen and stabilise the knee.
Anterior Cruciate Ligament (ACL) Non-operative treatment
Non-operative or “conservative” treatment may involve a physiotherapy programme to help rehabilitate the knee.
Strengthening exercises aim to build up other supporting muscles around the knee in an attempt to compensate for the deficient ACL. Once the power of the muscles has been restored balance and “proprioception” exercises are commenced. Proprioception exercises help to retrain positional sense and reflex pathways in the knee to try and prevent further instability.
Specially designed ACL knee braces can be used to provide extra support to the knee. These braces tend to be rather large and bulky and are often not well tolerated for long term use. Specialist advice is advised before investing in an expensive ACL brace.
Anterior Cruciate Ligament (ACL) Surgery
ACL reconstruction surgery is often performed in cases where conservative management has failed or is unlikely to provide sufficient knee stability.
ACL reconstruction is the commonest ligament reconstruction performed in the knee. It is a complex surgical procedure carried out to replace the torn ACL with an “artificial” structure called a graft.
The commonest types of graft used for this surgery are the “hamstring graft” and the “patella tendon graft”. These grafts are taken from other parts of the knee during surgery and engineered to form a new ACL- type structure.
Other less commonly used grafts include the quadriceps tendon, processed allografts (from cadavers) and man-made synthetic grafts.
Each type of graft tissue has its own potential benefits and problems. Generally hamstring and patella tendon grafts are considered to be the “gold standard”.
The surgery is usually performed arthroscopically and small incisions are used to harvest the graft used for the reconstruction.
The majority of reconstructions are performed as day case procedures, although occasionally an overnight stay is required.
It takes many months for the knee and new graft to build up strength after surgery and it is essential that sporting activities are not started too soon to help prevent re-rupture.
Physiotherapy advice and guidance is usually helpful to guide the rehabilitation process.


What are the risks of ACL reconstruction?
As with every procedure, there are some risks associated with ACL reconstruction. We have not included the chance of these happening as they are specific to you and differ for every person. Ask your surgeon to explain how these risks apply to you.
Side-effects
Side-effects are the unwanted but mostly temporary effects you may get after having the procedure.
After ACL reconstruction you may have side-effects, including:
- pain
- stiffness
- bruising and swelling
Complications
Complications are when problems occur during or after the operation. Most people aren’t affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, infection, excessive bleeding or developing a blood clot, usually in a vein in the leg (deep vein thrombosis, DVT).
The main complications of ACL reconstruction are listed below:
Tearing of the new graft used to reconstruct the ACL.
Numbness along the outside of your upper leg, near where the surgical cuts were made. This may be permanent.
Your knee joint may remain unstable. This can happen if the tendon used as the graft tears or stretches.
Stiffness in your knee, or less movement than you had before your injury.
Long-term knee pain, or pain when you kneel down.
Other Knee Ligament injuries
Minor injuries to supporting knee ligaments are common. This is usually in the form of a strain or sprain to the medial collateral ligament and can often be managed with “RICE” or bracing. Occasionally a collateral ligament can be pulled from its attachment onto the bone and may get lodged within the knee. This type of injury usually necessitates early repair.
Surgery for Damaged Knee Cartilage
The articular cartilage covering the bony surfaces may become damaged or torn following a knee injury. This type of injury is often associated with ligament tears or direct blows to the joint. Unfortunately the “hyaline” cartilage covering the bone has poor healing potential and often leaves areas of bone exposed or a thin layer of scar tissue which doesn’t work well.
If the area of cartilage injury is small or of only partial thickness, then symptoms may settle without any treatment or intervention. Small partial thickness flaps of cartilage may cause catching or crepitation symptoms in the knee and may be trimmed and smoothed using arthroscopic surgery.
If the area of cartilage damage is full thickness (down to the bone) this tends to cause more problems. Surgical techniques can be used to try and fill the gap in the cartilage with thicker, more durable tissue in an attempt to delay or prevent arthritis. Unfortunately the results of cartilage “regeneration & repair” techniques are not yet producing a surface as good as the original hyaline cartilage.
The more common procedures for cartilage restoration include:
- Microfracture
- Autologous Membrane Induced Chondrogenesis (AMIC)
- Autologous Chondrocyte Implantation (ACI)
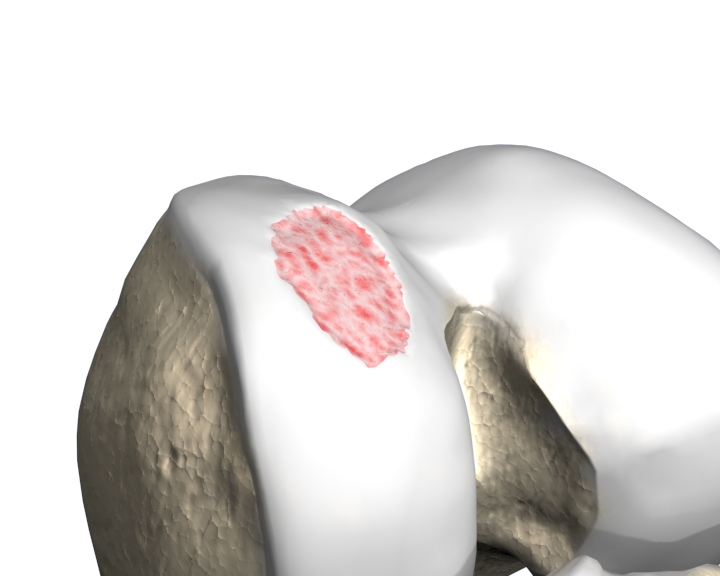
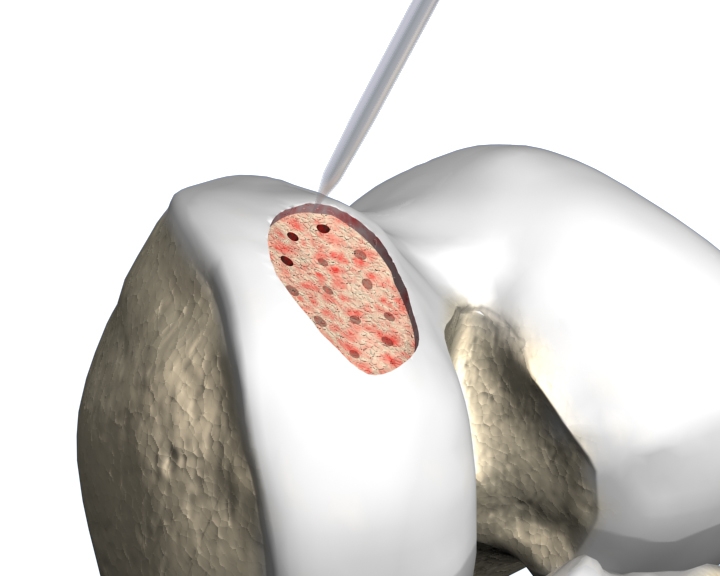
Microfracture
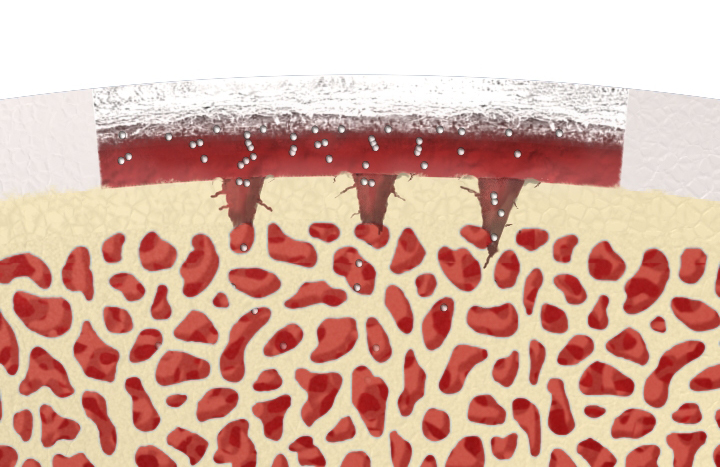
Microfracture is a surgical option used to treat smaller areas of damaged cartilage (not widespread arthritis). Microfracture is performed to stimulate new cartilage growth.
The Microfracture procedure involves the surgeon making multiple small holes into the bone where the cartilage is absent and allowing an influx of blood, rich in growth factors, to coat the bone surface. This forms a blood clot that over time develops into new cartilage, also known as fibrous cartilage. This fibrous cartilage helps protect the damaged joint – but is not as durable as the normal “hyaline” cartilage.
The Microfracture procedure is usually performed arthroscopically as a day case procedure or with an overnight stay.
The real key to treatment is appropriate rehabilitation following the surgery. Rehabilitation must protect the area treated by microfracture as well as maintain the strength and motion of the knee joint. The rehabilitation regimen depends upon the location and size of the area being treated.
The general principles of the rehabilitation for Microfracture are outlined below:
Protected Weight-Bearing – usually crutches are used for the first 6 weeks. The amount of weight put on the treated area must be limited. This allows the new cells to grow and develop. Crutches are used for the first 6 weeks reduce the force passing across the knee. If the microfracture has been carried out on the kneecap (patella) or within the groove for the patella (trochlea) then a knee brace may also be worn to prevent the knee bending more than 30 degrees.
Weight bearing is usually limited for 6 weeks, and then gradually increased over time. It may take 6 to 9 months before returning to sporting activities, and even longer to return to competition. Professional athletes may be sidelined up to a year after microfracture surgery.
Range-of-Motion – Range-of-motion is usually initiated early on after surgery. However, if the area of microfracture treatment is on the kneecap or within its groove, then motion will be limited for several weeks.
The aim is to restore full range of movement with minimal force passing through the joint. This can be achieved using a cycling machine on the lowest resistance setting or sitting with your foot on a skateboard and slowly bending and straightening the knee.
The reason for starting motion as early as possible is that the movement helps stimulate cartilage growth in the area of microfracture.
Autologous Membrane Induced Chondrogenesis (AMIC)
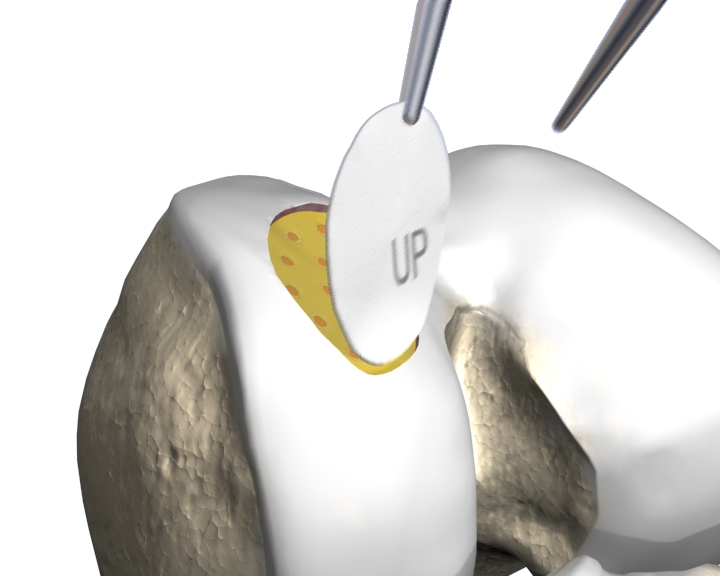
Autologous Matrix-Induced Chondrogenesis (AMIC) is a biological treatment option which can be used to treat cartilage damage. It combines microfracture surgery with the application of a complex membrane tissue made from collagen. The collagen membrane (Chondro-Gide, Geistlich Pharma AG, Switzerland) allows treatment of larger cartilage lesions that are not suitable for microfracture treatment alone.
The AMIC procedure is a minimally invasive, single step technique. Initially microfracture is performed to the area of damaged cartilage and unstable fragments of cartilage are removed. A protective Chondro-Gide membrane is then secured over the treated area. The protective membrane helps encourage the migration of new cells into the injured area and protects the developing cartilage tissue.
The rehabilitation following AMIC surgery is very similar to that of microfracture. For the first 2 days the knee is usually kept straight in a knee brace and then range of movement exercises are commenced. As with microfracture, weight needs to be kept off the knee for the first six weeks.
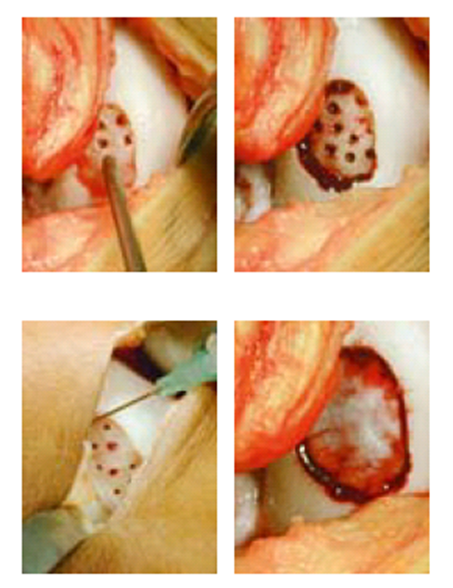
Autologous Chondrocyte Implantation (ACI)
ACI is a biological treatment used to treat larger cartilage defects. It is not used to treat generalised arthritis or “wear and tear” in the knee. Suitable patients would be generally young and healthy individuals, who have had an injury to the knee over the past few months or years, and have on-going pain, swelling and mechanical problems. Although cartilage damage is often associated with ligament and meniscal injuries, it is important that the knee is stable and that there are no major alignment problems, prior to cartilage repair.
ACI requires two surgical procedures. Initially healthy cartilage cells (chondrocytes) are harvested using arthroscopic surgery from a non-weight bearing part of the knee and sent away to be grown in a laboratory for approximately 6-8 weeks. A second (more invasive) procedure is then used to re-implant the “new” cartilage cells into the damaged area.
Over time the new cartilage cells begin to produce protective cartilage in the damaged area. This new cartilage is not “normal” – but may be more protective in the longer term than the scar tissue formed following microfracture.
As with all the treatments used manage cartilage injuries the rehabilitation protocol is critical. You will be guided through this process by your surgeon and physiotherapist.
As the swelling within the joint subsides and the range of movement returns symptoms of instability may develop. This is often described as the joint feeling vulnerable during particular activities or may present as “giving-way” and collapse of the joint.
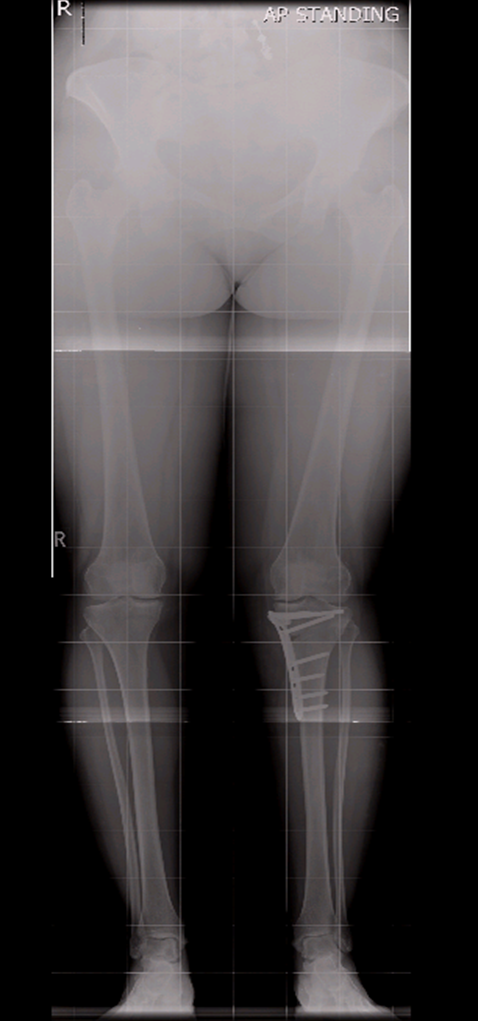
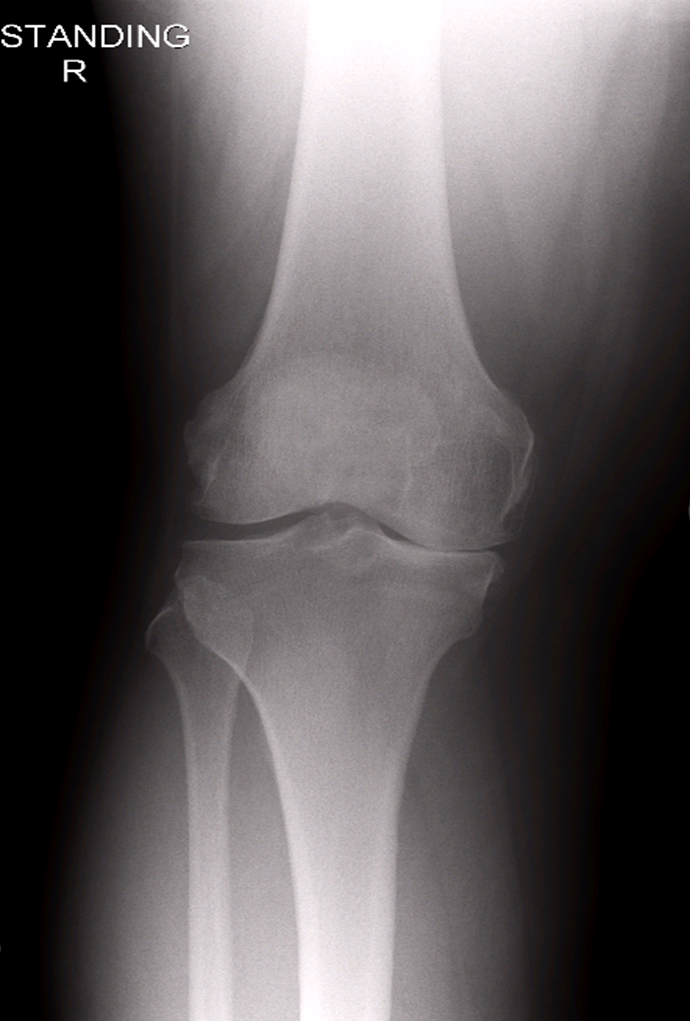
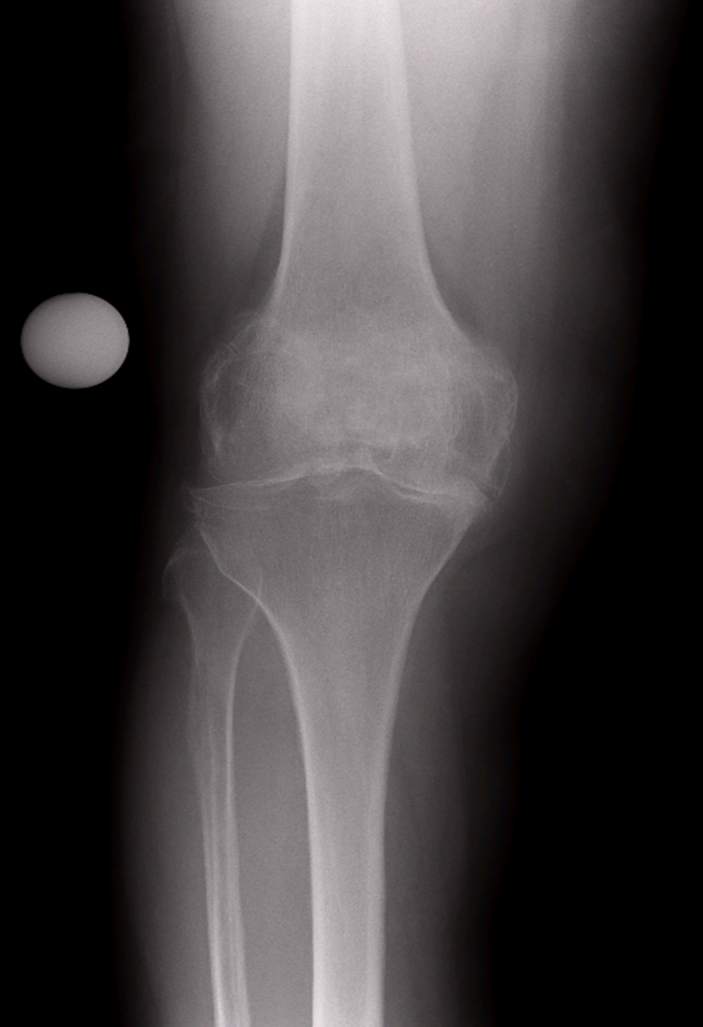
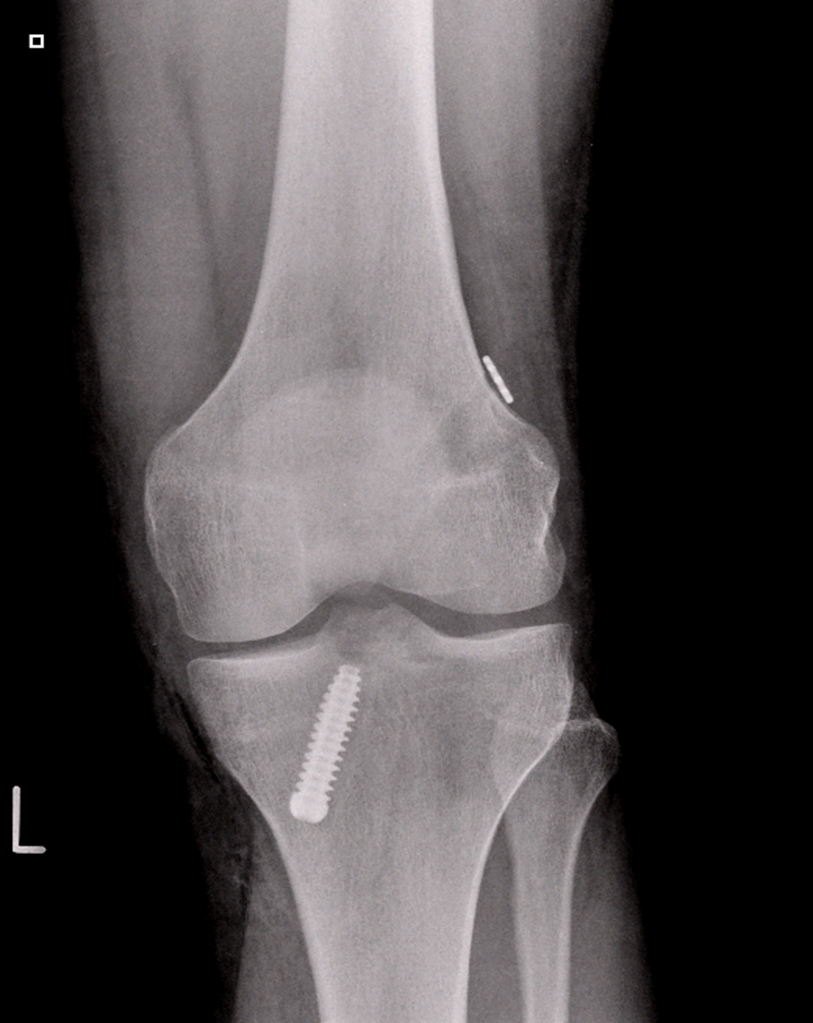
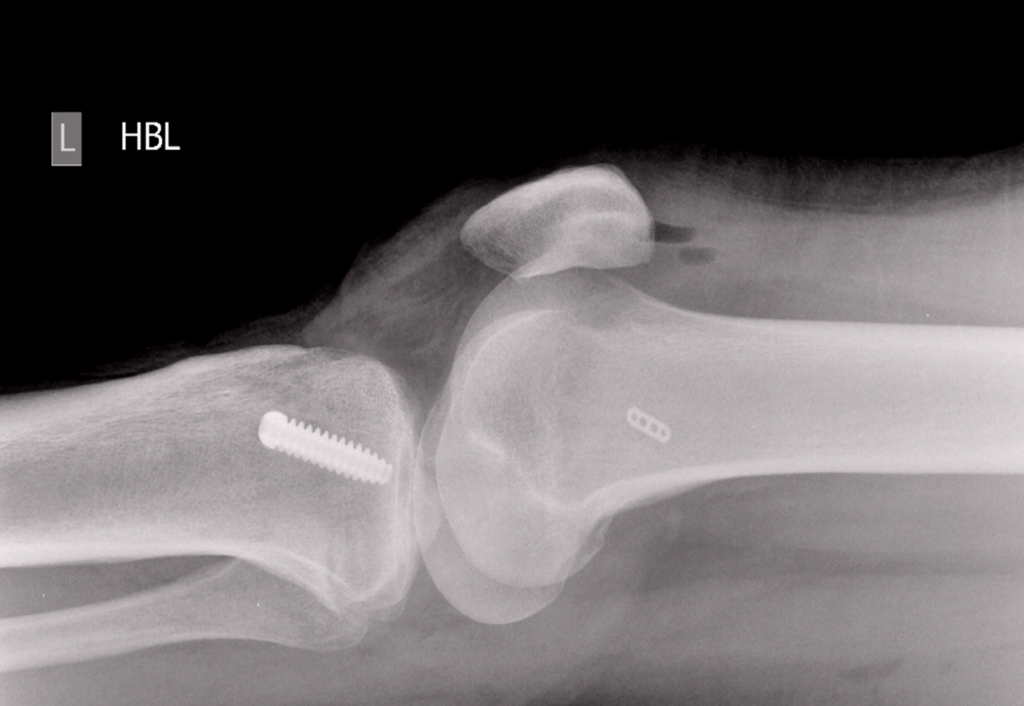
Surgery for Knee Arthritis
Knee arthritis develops when a part (or all) of the cartilage covering the knee joint wears away. Typically this occurs in older people as years of activity, hard work or sporting injuries begin to take their toll. Occasionally arthritis develops in younger people as a result of injury, genetic susceptibility or just bad luck.
Once arthritis is established the main surgical options include:
- Osteotomies – to realign the joint
- Partial knee replacement – replacing the worn section and leaving the “good bits” alone
- Total knee replacement
Osteotomies are performed to change the way forces pass through the joint. They are used to try and move pressure away from damaged parts of the knee to help protect them. Osteotomies are usually performed in the lower femur (thigh bone) or upper tibia (shin bone). After cuts have been made, the bone is carefully repositioned using X-ray guidance and then the new position fixed with metal plates and screws. Occasionally osteotomies are used to help protect damaged ligaments and help improve knee stability.
Following surgery most patients are ready to go home within 48 hours. The plate and screws are made of titanium and are very strong so you can partially bear weight on the operated leg straight away with the help of crutches. It is normal for the operated leg to be rather swollen and bruised for several weeks after this procedure. Regular icing, elevation and gentle range of movement exercises are used to help reduce the swelling (and pain)
After six weeks, if the x-rays show the bone is healing well you can progress to full weight bearing and dispense with your crutches as the discomfort settles. It usually takes many months for the osteotomy site to fully heal and for the leg pain to completely settle. Occasionally the metal plates securing the osteotomy may need to be removed once the bone has healed as they may cause irritation.
What are the risks of knee osteotomy surgery?
- Deep vein thrombosis and pulmonary embolus: A combination of surgery, immobilisation of the limb, smoking and the oral contraceptive pill or hormonal replacement therapy all multiply to increase the risk of a blood clot. Any past history of blood clots should be brought to the attention of the surgeon prior to your operation. The oral contraceptive pill, hormonal replacement therapy and smoking should cease one week prior to surgery to minimise the risk. Blood thinning injections will be given following your surgery to help reduce the chance of developing a clot
- Excessive bleeding resulting in a haematoma is known to occur with patients taking aspirin or anti-inflammatory drugs. They should be stopped at least one week prior to surgery.
- Infection: Surgery is carried out under strict germ free conditions in an operating theatre. Antibiotics are administered intravenously at the time of your surgery. Any allergy to any known antibiotics should be brought to the attention surgeon or anaesthetist. Despite these measures, following surgery there is a less than 3% chance of developing an infection. Most commonly these are superficial wound infections that resolve with a course of antibiotics. More serious infections may require further hospitalisation and treatment.
- Nerve Injury: Injury to the peroneal nerve can occur in patients following knee osteotomy. This may result in sensory loss or muscle weakness in the lower leg. Very rarely this weakness may be permanent and lead to a “foot-drop” problem.
- Injury to the blood vessels around the knee during surgery is a very rare complication (less than 1%).
- Delayed or non-union of the osteotomy (failure to heal) site may occur in 2 to 4% of cases. Further surgery may be required if this occurs. The risk of non-union is far higher in smokers and this type of surgery is generally contra-indicated in people who smoke.
- Further surgery: over time the “healthy” areas of the knee joint may also wear out and become arthritic. In this situation a Total Knee Replacement is usually needed. Total knee replacement following a knee osteotomy is a technically more difficult procedure than if no osteotomy has been performed.
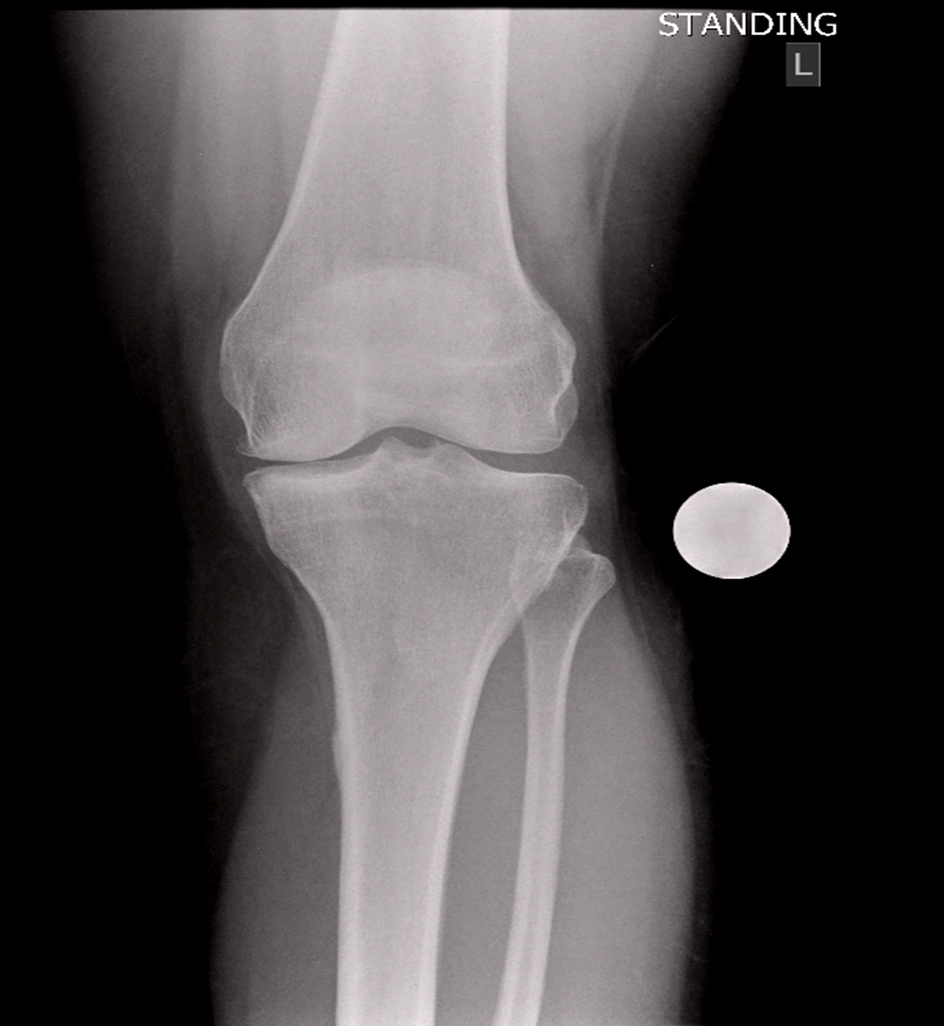
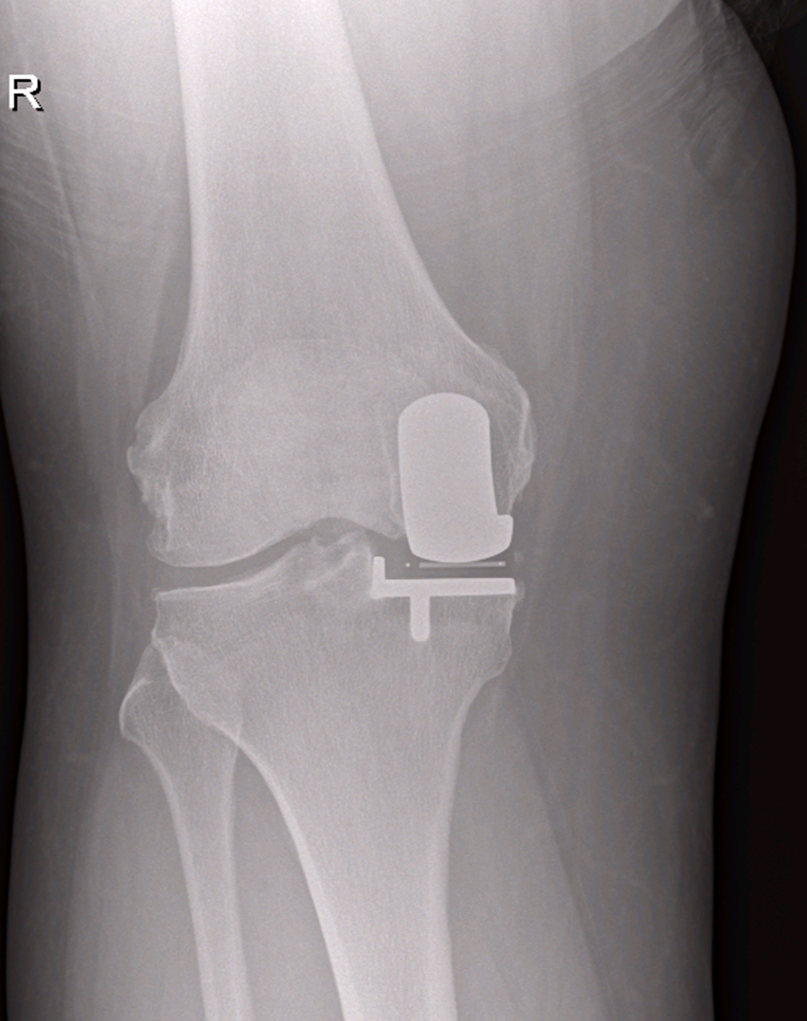
Partial Knee Replacement
Partial knee replacement surgery can be performed in painful arthritic knees that are no longer helped with non-surgical treatments. Partial knee replacement is carried out to treat arthritis that is isolated to one weight bearing region of the knee. The surgery removes the surface of the joint in the diseased area, but leaves the healthy (non-arthritic) parts of the knee alone. The most commonly performed partial knee replacements are used to treat arthritis in the medial (inside) half of the joint or arthritis behind the patella.
For a partial knee replacement to work well the non-diseased weight bearing parts of the joint need to be in good condition and the knee ligaments need to be stable – this situation arises in approximately 30% of arthritic knees.
The potential advantages of partial knee replacement (compared with a conventional knee replacement) are:
- Smaller incisions and less bone removed
- Shorter length of hospital stay
- Faster mobilisation and recovery
- Improved range of movement after the surgery
- Reduced risk of blood clots & infection
- A more “normal” feeling knee with better function
The disadvantages of partial knee replacement (compared with total knee replacement) are:
- The other “normal” parts of the knee can wear out in time
- The chance of needing a revision (new replacement) or further surgery is higher with partial knee replacement compared with a total knee replacement
Your doctor will discuss the suitability of partial & total knee replacement surgery with you if joint replacement surgery is deemed necessary.
The surgery and hospital stay
You will be admitted on the same day as your operation.
The surgery is usually performed using a regional (spinal) anaesthetic with sedation or a general anaesthetic. The operation takes 1-2 hours. At the time of the surgery your surgeon will have a good look around the inside part of your knee. If the arthritis is isolated to one weight-bearing region then the partial knee replacement will be performed. If there appears to be significant wear or damage in other parts of the knee – or if the ligaments inside the knee are not working, your surgeon will perform a Total Knee Replacement instead of the Partial Knee replacement (you will not be woken up to be told this but will be informed after the procedure!)
The knee implants are securely fixed in place and bending the knee should start immediately after the surgery. Normally you will be up walking on your knee the same day as your surgery with the help of a physiotherapist. The knee is often far more sore the day after the surgery and you will be given regular pain killers to help with this. It is important to ice the knee frequently to help reduce the swelling and keep it elevated when you are not up and around.
Usually you will be ready to go home 2 days after your surgery (some patients go home the day after surgery, some a few days later). At home it is vital that you continue with the regular pain killers, icing and exercise regimen –this helps to improve the range of movement and help reduce the swelling.
Following any form of knee replacement (partial or total) it is normal for the knee to continue to be uncomfortable, swollen and warm for up to 3 months after surgery. After this time the swelling gradually subsides and life gets easier! It usually takes 12 to18 months for all the improvement to be felt in the knee following partial or total replacement.
What are the risks of Partial Knee Replacement?
Partial knee replacement surgery is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
Side-effects
These are the unwanted, but mostly temporary effects of a successful treatment, for example feeling sick as a result of the anaesthetic.
Your knee will feel sore and stiff and may be swollen for up to six months.
You will have a scar over the front of the knee. You may not have any feeling in the skin around your scar. This can be permanent, but could improve over one to two years. The scar may be uncomfortable to kneel on.
Complications
This is when problems occur during or after the operation. Most people are not affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (DVT).
Specific complications of knee replacement are uncommon, but can include those listed below.
- Infection of the wound or joint. Antibiotics are given during and after surgery to help prevent this.
- Unstable joint. Your knee joint may become loose and you may require further surgery to correct this.
- Dislocation of bearing – the plastic bearing that separates the metal implants may slip out of place – usually as a result of a large twisting injury to the knee
- Damage to nerves or blood vessels. This is usually mild and temporary.
- Scar tissue. This can build up and restrict your movement. Further surgery may be needed to correct this.
- On-going pain – some patients continue to suffer pain in their knee despite replacement surgery
The artificial knee joint usually lasts for over 10 years. Over time it may begin to wear out or become loose (just like any other mechanical device) after which you may need to have it replaced.
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your surgeon to explain how these risks apply to you.
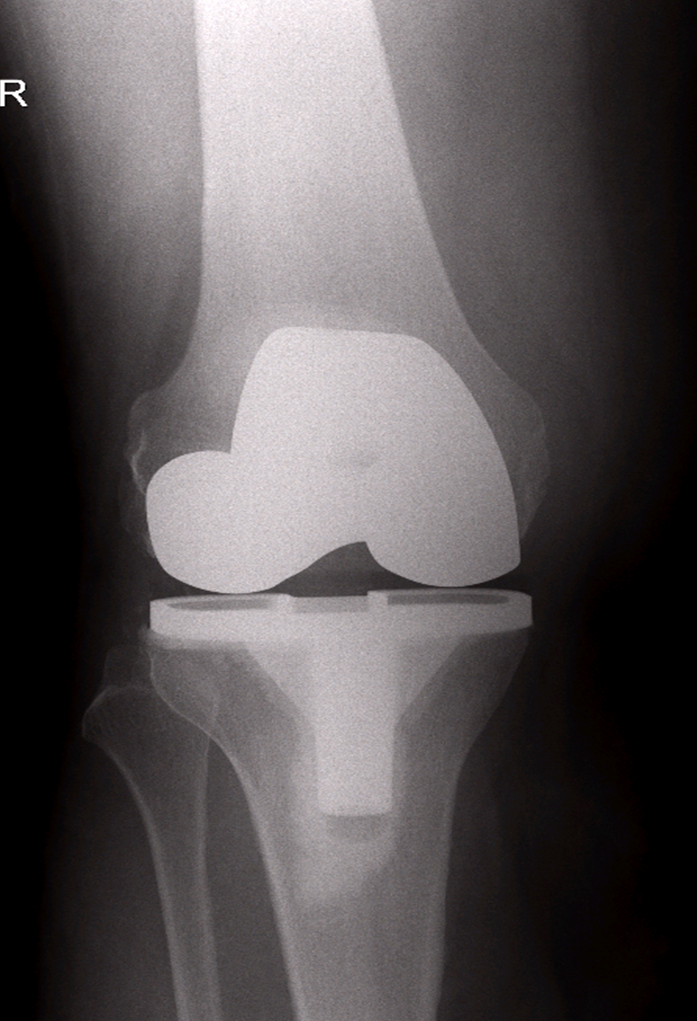
Total Knee Replacement
Total knee replacement surgery can be performed in painful arthritic knees that are no longer helped with non-surgical treatments. Total knee replacement is carried out to treat arthritis in any area of the joint – especially if more than one area of the knee is arthritic. The surgery removes the surface of the joint – replacing it with metal and plastic. In some circumstances the back part of the patella may also be resurfaced with plastic.
The surgery and hospital stay
You will be admitted on the same day as your operation.
The surgery is usually performed using a regional (spinal) anaesthetic with sedation or a general anaesthetic. The procedure usually takes 1-2 hours.
The knee implants are securely fixed in place and bending the knee should start immediately after the surgery. Normally you will be up walking on your knee the same day as your surgery with the help of a physiotherapist. The knee is often far more sore the day after the surgery and you will be given regular pain killers to help with this. It is important to ice the knee frequently to help reduce the swelling and keep it elevated when you are not up and around.
Usually you will be ready to go home 3 days after your surgery (some patients go home sooner, some a few days later). At home it is vital that you continue with the regular pain killers, icing and exercise regimen – this helps to improve the range of movement and help reduce swelling.
Following any form of knee replacement (partial or total) it is normal for the knee to continue to be uncomfortable, swollen and warm for 3 months after surgery. After this time the swelling gradually subsides and life gets easier! It usually takes 12 to18 months for all the improvement to be felt in the knee following a total replacement.
The amount of movement (bending) that can be achieved following knee replacement surgery is largely determined by how well the joint moved prior to surgery. This is one of the reasons why it is important to perform stretching and strengthening exercises both before and after surgery.
Total (and partial) knee replacements are made from metal and plastic it is not unusual to experience clicking sensations or sounds originating from knee – this is usually nothing to be concerned about and is a result of the metal and plastic bearings knocking together. Many patients also describe an intermittent ache (usually on the inside of the knee) that tends to be worse in the cold, wet weather – this usually improves over time and settles with simple pain killers.
What are the risks of Total Knee Replacement?
Total knee replacement surgery is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.
Side-effects
These are the unwanted, but mostly temporary effects of a successful treatment, for example feeling sick as a result of the anaesthetic.
Your knee will feel sore and stiff and may be swollen for up to six months.
You will have a scar over the front of the knee. You may not have any feeling in the skin around your scar. This can be permanent, but could improve over one to two years. The scar may be uncomfortable to kneel on.
Complications
This is when problems occur during or after the operation. Most people are not affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (DVT) or rarely in the lung (Pulmonary Embolism).
Specific complications of knee replacement are uncommon, but can include those listed below.
- Infection of the wound or joint. Antibiotics are given during and after surgery to help prevent this.
- Unstable joint. Your knee joint may become loose and you may require further surgery to correct this.
- Damage to nerves or blood vessels. This is usually mild and temporary.
- Scar tissue. This can build up and restrict your movement. Further surgery may be needed to correct this.
- On-going pain – some patients continue to suffer pain in their knee despite replacement surgery.
- The artificial knee joint usually lasts for well over 10 years. Over time it may begin to wear out or become loose (just like any other mechanical device) after which you may need to have it replaced.
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your surgeon to explain how these risks apply to you.
Get News & Updates
Stay in the loop with Northampton Orthopaedics with our latest news, events and advice.
What Patients Say